
SMALLPOX
The only human disease to be eradicated in human history thanks to vaccines. The last naturally occurring case was diagnosed in October 1977, and the World Health Organisation (WHO) certified the global eradication of the disease in 1980. It was one of the most devastating diseases known to humanity and caused millions of deaths before it was eradicated.

SARS
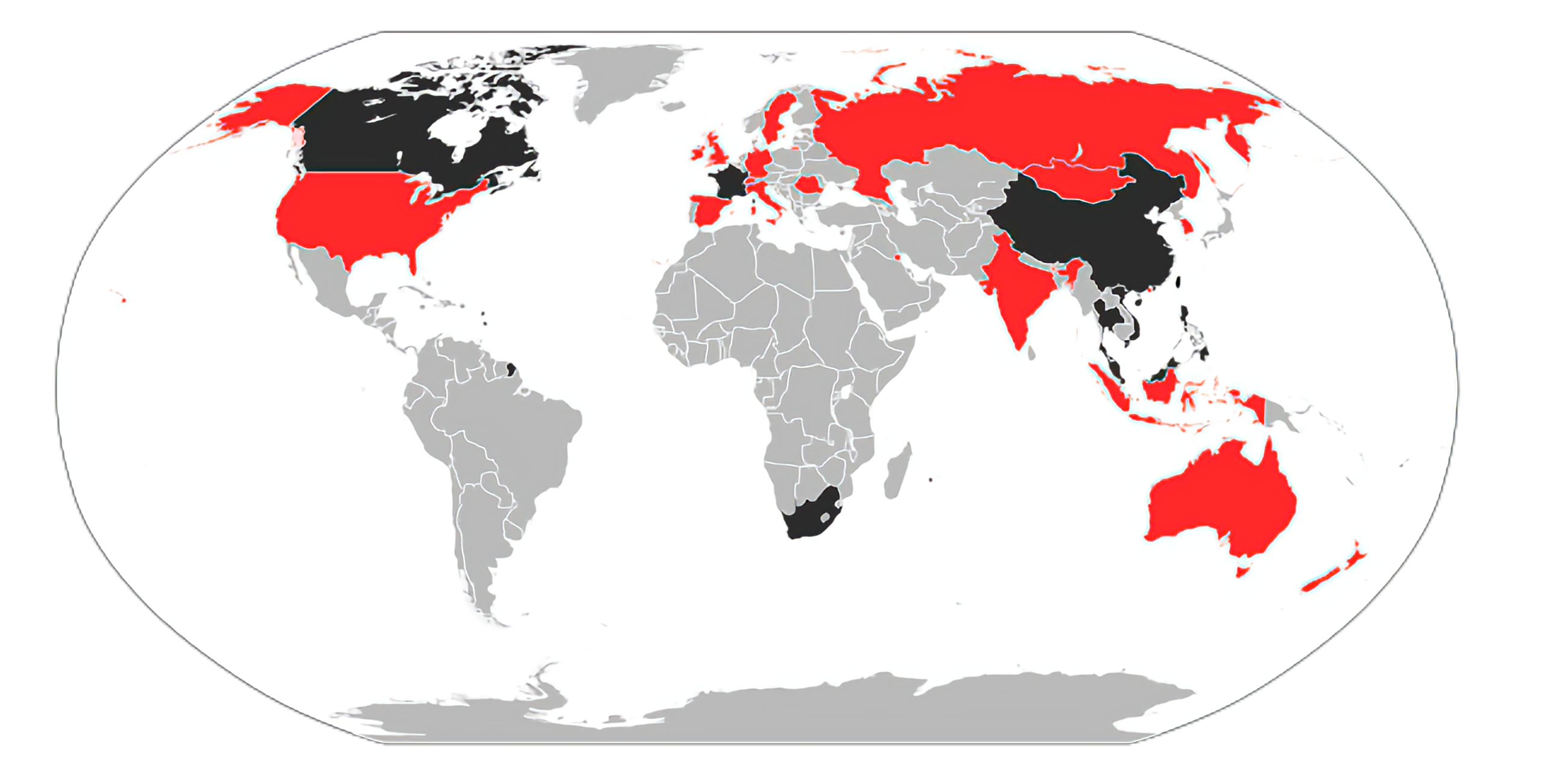
The first severe and readily transmissible new disease to emerge in the 21st century. It was first identified in November 2002 during an outbreak that emerged in China and spread to 29 other territories. A global alert was issued in March 2003 by WHO. On 5 July 2003, WHO declared SARS contained although several cases were reported until May 2004.
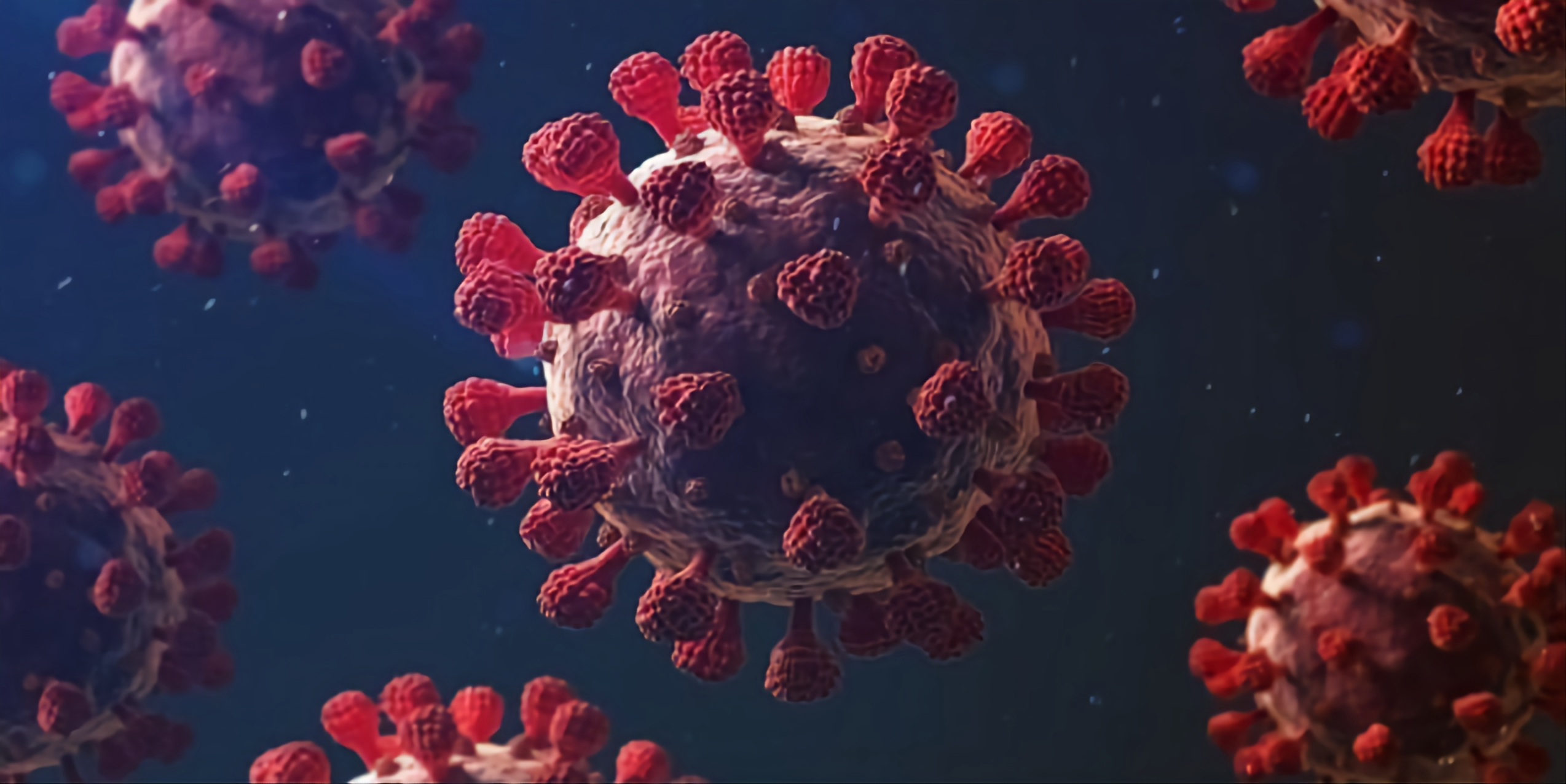
COVID-19
The first known case was identified in Wuhan, China in December 2019. The disease quickly spread worldwide, resulting in the COVID-19 pandemic. It’s caused by the coronavirus, the same type of virus that brought SARS in 2002. Likely originated in animals before they were transmitted to humans by an intermediate host.

INFLUENZA (FLU)
A contagious respiratory illness caused by influenza viruses that infect the nose, throat, and lungs. Since recorded, influenza has caused major global outbreaks at unpredictable intervals. Of these pandemics, the "Spanish flu" in 1918 was the most severe, causing an estimated 20-40 million or more deaths worldwide; less severe pandemics occurred in 1957 and 1968.

RABIES
Rabies is present on all continents, except Antarctica, with over 95% of human deaths occurring in the Asia and Africa regions. Dogs are the main source of human rabies deaths, contributing up to 99% of all rabies transmissions to humans. The rabies virus infects the central nervous system of mammals, ultimately causing disease in the brain and death.
What is Virus?
Viruses are not cellular organisms
Viruses do not have a cellular structure
Viruses require a host cell to make new products
The virus does not carry out any life process outside of a cell. Nonetheless, viruses reproduce using living cells by injecting their genetic materials into host cells.
Viruses are made up of nucleic acid (DNA or RNA)
The size of a virus is very small (20 nm to 400 nm), therefore virus cannot be seen using a light microscope but can only be seen using an electron microscope.
Awareness
Uncontrolled environmental devastation caused by humans is causing harm to every species. In these thousands of years of ‘war’ between humans and viruses, the younger the virus, the less we know about it, and the more helpless we are to combat it. Known viruses currently are not the vital threat to us right now, but instead a newly revolved virus in near future with a high fatality rate, high transmission rate and long incubation period. Hence, we should minimise the threats by taking precautions on forthcoming possible threats of newly emerging viruses before they appear.

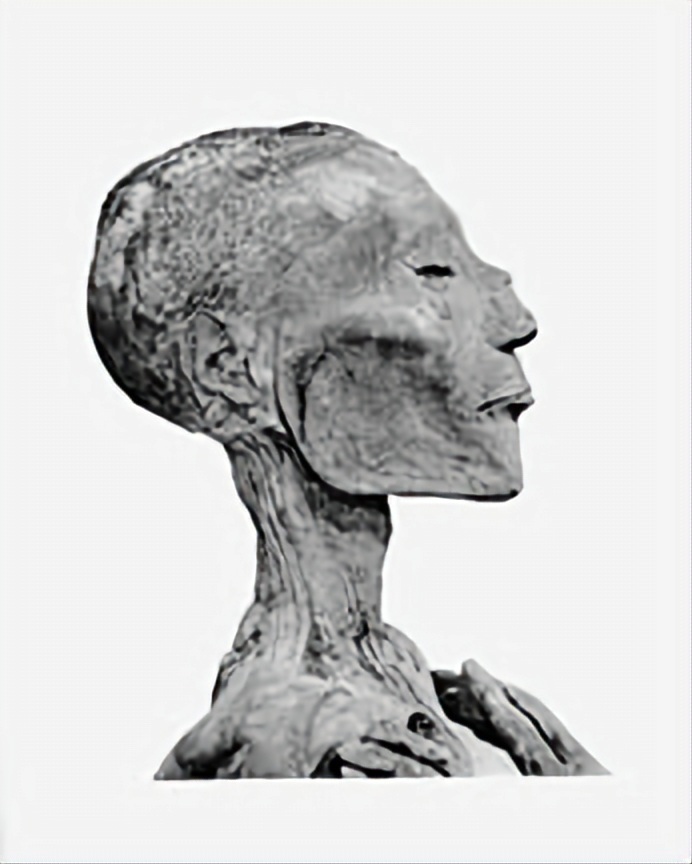
SMALLPOX
The only human disease to be eradicated in human history thanks to vaccines. The last naturally occurring case was diagnosed in October 1977, and the World Health Organisation (WHO) certified the global eradication of the disease in 1980. It was one of the most devastating diseases known to humanity and caused millions of deaths before it was eradicated.
Background
Status: Eradicated (1980)
First discovered: Unknown
Existence: At least 3000 years
Origin: Unknown
Outbreak: -
Frequency: -
Deaths: -
Causes
☣
Pathogen
Virus: Variola virus
Variants: Variola major & Variola minor
⚗
Transmission
Type of transmission: Airborne & Through Contact
Transmitted through: Respiratory droplets, coughing, sneezing, face-to-face contact, contaminated objects/ surfaces
Signs and Symptoms
Incubation Period: 7 - 17 days
Initial Symptoms
(2-4 days):
◉ High fever
◉ Fatigue
◉ Severe back pain
◉ Less often, abdominal pain and vomiting
Rash
(Lasts about 4 days):
1. Rash (small red spots) begins on the face and hands, then spreads to the rest of the body
2. Fever begins to decline
3. Skin sores fill with a thick, opaque fluid and often have a dent in the centre
Pustular Rash and Scabs
(Lasts about 10 days):
1. Sores become pustules
2. Pustules begin to form a crust and then scab
Scabs Fall Off
(Lasts about 6 days):
The scabs begin to fall off, leaving marks on the skin
No Scabs
(After 4 weeks):
Once all scabs have fallen off, the person is no longer contagious
Diagnosis
◉ Fever >= 38.3 °C
◉ Rash characteristic
◉ Confirmed using laboratory test, PCR
Prevention and Treatment
Treatment: Antiviral Drugs
In July 2018, Food and Drug Administration (FDA) approved tecovirimat, the first drug approved for treatment of smallpox
Supportive care
◉ Aimed at reducing the signs and symptoms for the comfort and well-being of the patient
◉ No treatments available
Vaccination
Smallpox vaccine: Vaccinia virus was used
Immunity period: 3 - 5 years
◉ Smallpox was the first disease to be prevented by vaccination, discovered by Edward Jenner, a doctor in England, in 1796
◉ Vaccination for the general population is no longer recommended because the disease has been eradicated
Prognosis and Complications
Prognosis
◉ Variola major: 30% mortality rate
◉ Variola minor: 1% mortality rate
Complications
◉ Survivors bore the scars of the disease for life
◉ If the eye was infected, blindness was common.
◉ Respiratory complications
◉ Death
History
Disease Emergence
◉ 3rd Century BCE—Mummies from ancient Egypt showed evidence of infection
◉ 4th Century—Earliest written description of a disease like smallpox appeared in China
◉ 6th Century—Increased trade with China and Korea brings smallpox to Japan.
◉ 7th Century—Arab expansion spreads smallpox into northern Africa, Spain, and Portugal.
◉ 11th Century—Crusades further spread smallpox in Europe.
◉ 15th Century—Portugal occupies part of western Africa, bringing smallpox.
◉ 16th Century—European settlers and the African slave trade import smallpox into the Caribbean & Central and South America
◉ 17th Century—European settlers bring smallpox to North America.
◉ 18th Century—Explorers from Great Britain bring smallpox to Australia.

Early Control Efforts
◉ Variolation (Exposure to material from smallpox sores (pustules) by scratching the material into their arm or inhaling it through the nose to protect against smallpox)
◉ Vaccination began in 1796 when the English doctor Edward Jenner noticed that milkmaids who had gotten cowpox were protected from smallpox. To test his theory, Dr. Jenner took material from a cowpox sore on milkmaid Sarah Nelmes’ hand and inoculated it into the arm of James Phipps, the 9-year-old son of Jenner’s gardener. Months later, Jenner exposed Phipps several times to variola virus, but Phipps never developed smallpox.
◉ Vaccination became widely accepted and gradually replaced the practice of variolation
◉ The virus used to make the smallpox vaccine changed from cowpox to vaccinia virus in the 1800s
Last Cases of Smallpox
◉ In late 1975, three-year-old Rahima Banu from Bangladesh was the last person in the world to have naturally acquired variola major. An 8-year-old girl named Bilkisunnessa reported the case to the local Smallpox Eradication Program team and received a 250 Taka reward
◉ The 1978 smallpox outbreak in the United Kingdom resulted in the death of Janet Parker, a British medical photographer at England’s Birmingham University Medical School, who became the last recorded person to die from smallpox.

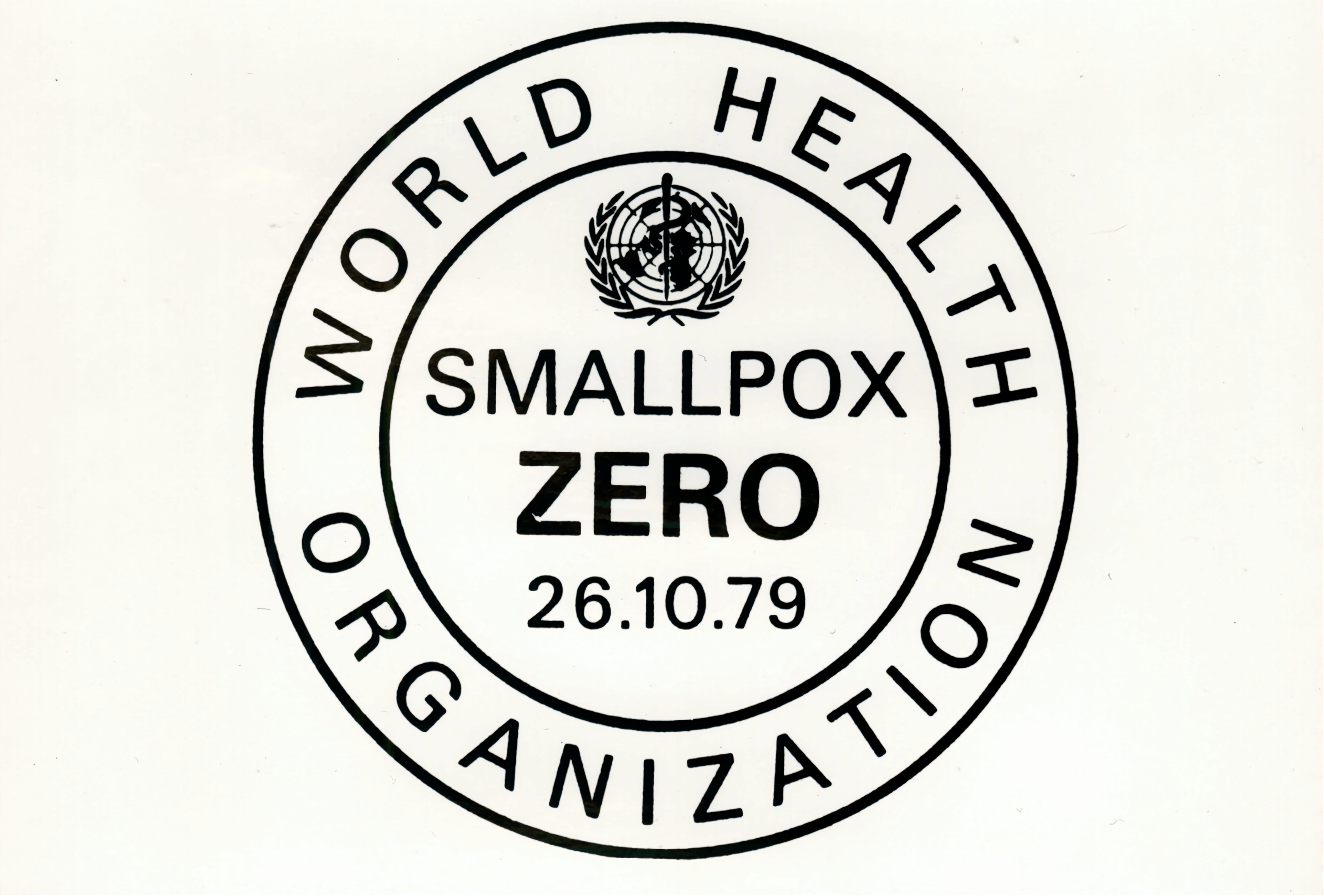
Eradication
◉ World Health Assembly (WHO) declared the world free of this disease on May 8, 1980

SARS
The first severe and readily transmissible new disease to emerge in the 21st century. It was first identified in November 2002 during an outbreak that emerged in China and spread to 29 other territories. A global alert was issued in March 2003 by WHO. On 5 July 2003, WHO declared SARS contained although several cases were reported until May 2004.
Background
Status: No cases reported since 2004
First discovered: November 2002
Existence: 20 years
Origin: Shunde, Guangdong, China
Outbreak: 2002–2004 SARS Outbreak
Frequency: 8096 cases
Deaths: 783 known
Causes
☣
Pathogen
Virus: Severe acute respiratory syndrome coronavirus (SARS-CoV-1)
Species: SARS-related coronavirus
⚗
Transmission
Type of transmission: Airborne & Through Contact
Transmitted through: Respiratory droplets of saliva, coughing, sneezing, contaminated objects/ surfaces
Signs and Symptoms
Incubation Period: 2 - 7 days
Initial Symptoms:
◉ High fever (>38 °C)
◉ Headache
◉ Malaise
◉ Muscle pain
◉ Lethargy
◉ Cough
◉ Sore
After 3-7 days:
1. Dyspnoea (shortness of breath) (require intubation and mechanical ventilation if severe)
2. Hypoxemia (low blood oxygen levels)
3. White blood cell count is often decreased early in the disease
4. Low platelet counts at the peak of the disease
5. Pneumonia (inflammatory condition of the lung)
Diagnosis
◉ Any of the symptoms
◉ Fever >= 38 °C
◉ Tested positive for SARS using ELISA or PCR
◉ Either a history of:
Contact with someone with a diagnosis of SARS within the last 10 days
or
Travel to any of the regions identified as areas with recent local transmission of SARS
Prevention and Treatment
Prevention
◉ Hand-washing with soap and water, or use of alcohol-based hand sanitizer
◉ Disinfection of surfaces of fomites to remove viruses
◉ Avoiding contact with bodily fluids
◉ Avoiding travel to affected areas
◉ Wearing masks and gloves
◉ Isolation of suspected of probably cases
◉ Quarantine of suspected contacts for 10 days
Supportive care
◉ Aimed at reducing the signs and symptoms for the comfort and well-being of the patient
◉ No treatments available
◉ With antipyretics (a substance that reduces fever), supplemental oxygen and mechanical ventilation as needed
◉ Must be isolated, preferably in negative-pressure rooms
Antiviral Drugs & Vaccination
◉ None available
Prognosis and Complications
Prognosis
◉ 9.5% mortality rate
Complications
◉ Acute respiratory distress syndrome (ARDS)
◉ Death
History
Outbreak in South China
◉ The SARS epidemic began in the Guangdong province of China on 16 November 2002. The index patient, a farmer from Shunde, Foshan, Guangdong, was treated in the First People's Hospital of Foshan. The patient died soon after, and no definite diagnosis was made on his cause of death. Despite taking some action to control it, Chinese government officials did not inform the World Health Organisation (WHO) of the outbreak until February 2003 which caused delays in efforts to control the epidemic.

Spread to other regions
◉ The epidemic reached the public spotlight in February 2003, when an American businessman travelling from China, Johnny Chen, became affected by pneumonia-like symptoms while on a flight to Singapore. The plane stopped in Hanoi, Vietnam, where the patient died in Hanoi French Hospital. Several of the medical staff who treated him soon developed the same disease despite basic hospital procedures.
◉ Local transmission of SARS took place in Toronto, Ottawa, San Francisco, Ulaanbaatar, Manila, Singapore, Taiwan, Hanoi and Hong Kong whereas within China it spread to other provinces. It spreaded to 30 countries or regions in the end.
Identification of virus
◉ Italian doctor Carlo Urbani identified the threat and communicated it to WHO and the Vietnamese government; he later died from the disease.
◉ On 12 March 2003, WHO issued a global alert.


Containment
◉ The World Health Organisation (WHO) declared SARS contained on 5 July 2003. In the following months, only four SARS cases were reported in China between December 2003 and January 2004.
COVID-19
The first known case was identified in Wuhan, China in December 2019. The disease quickly spread worldwide, resulting in the COVID-19 pandemic. It’s caused by the coronavirus, the same type of virus that brought SARS in 2002. Likely originated in animals before they were transmitted to humans by an intermediate host.
Background
Status: Pandemic
First discovered: December 2019
Existence: 3 years
Origin: Wuhan, China
Outbreak: COVID-19 pandemic (2019 - present)
Frequency: 612,052,035 confirmed cases (As of 19 Sept 2022)
Deaths: 6,526,618 (As of 19 Sept 2022)
Causes
☣
Pathogen
Virus: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
Species: SARS-related coronavirus
Variants: Alpha, Beta, Delta, Gamma, and Omicron
⚗
Transmission
Type of transmission: Airborne & Through Contact
Transmitted through: Respiratory droplets/ aerosols, breathing, talking, coughing, sneezing, contaminated objects/ surfaces
Signs and Symptoms
Incubation Period: 2 - 14 days
Mild Symptoms
◉ Fever
◉ Cough
◉ Fatigue
◉ Muscle or body aches
◉ Headache
◉ Loss of taste or smell
◉ Sore throat
◉ Congestion or runny nose
◉ Nausea or vomiting
◉ Diarrhoea
Moderate Symptoms:
1. Shortness of breath
2. Pneumonia (inflammatory condition of the lung)
Severe Symptoms
(Hospitalisation required):
1. Dyspnea (Shortness of Breath)
2. Hypoxia (Inadequate oxygen supply at the tissue level)
Critical Symptoms
(ICU admission required):
1. Respiratory failure
2. Septic shock
3. Multiorgan dysfunction
Diagnosis
◉ Any of the symptoms
◉ Chest CT scans
◉ Tested positive for COVID-19 using NAATs (PT-PCR) or Antigen tests
Prevention and Treatment
Prevention
◉ Vaccination
◉ Wear a mask in public
◉ Avoid crowded places
◉ Physical/ physical distancing
◉ Indoor ventilation
◉ Hand-washing and hygiene
◉ Self-isolation
◉ Quarantine for 14/10 days
◉ International travel-related control measures
Supportive care
◉ Aimed at reducing the signs and symptoms for the comfort and well-being of the patient
◉ No specific, effective treatments available although several medications have been approved in different countries
◉ Medication
◉ Hospitalisation
◉ ICU admission
◉ Mechanical ventilation
Vaccination
COVID-19 vaccine: Replication-incompetent adenovirus type 26 expressing the SARS-CoV-2 spike protein/ mRNA of the virus was used
Immunity period: At least 6 months
◉ In 2020, the first COVID-19 vaccines were developed and made available to the public
◉ Most COVID-19 vaccines were two-dose vaccines
Prognosis and Complications
Prognosis
◉ 3 - 4% of the cases are severe enough to cause hospitalisation
◉ Mild cases typically recovered within two weeks
◉ Severe or critical cases may take three to six weeks to recover
◉ 1.1% case fatality rate (CFR) as of 13 August 2022
Complications
◉ Pneumonia (inflammatory condition of the lung)
◉ Acute respiratory distress syndrome (ARDS)
◉ Multi-organ failure
◉ Septic shock
◉ Seizure
◉ Stroke
◉ Death
Longer-term effects
◉ Fatigue
◉ Shortness of breath
◉ Loss of taste or smell
◉ Headache
◉ Sleep problems
◉ Brain fog (Difficulty thinking or concentrating)
History
First identified cases
◉ The first confirmed human infections were in Wuhan. Human-to-human transmission was confirmed by the WHO and Chinese authorities by 20 January 2020. There are several theories about where the index case originated and investigations into the origin of the pandemic are ongoing. According to official Chinese sources, these were mostly linked to the Huanan Seafood Wholesale Market, which also sold live animals.


Outbreak
◉ In early and mid-January 2020, the virus spread to other Chinese provinces, helped by the Chinese New Year migration and Wuhan being a transport hub and major rail interchange. On 30 January, the WHO declared COVID-19 a Public Health Emergency of International Concern. By this time, the outbreak had spread by a factor of 100 to 200 times.
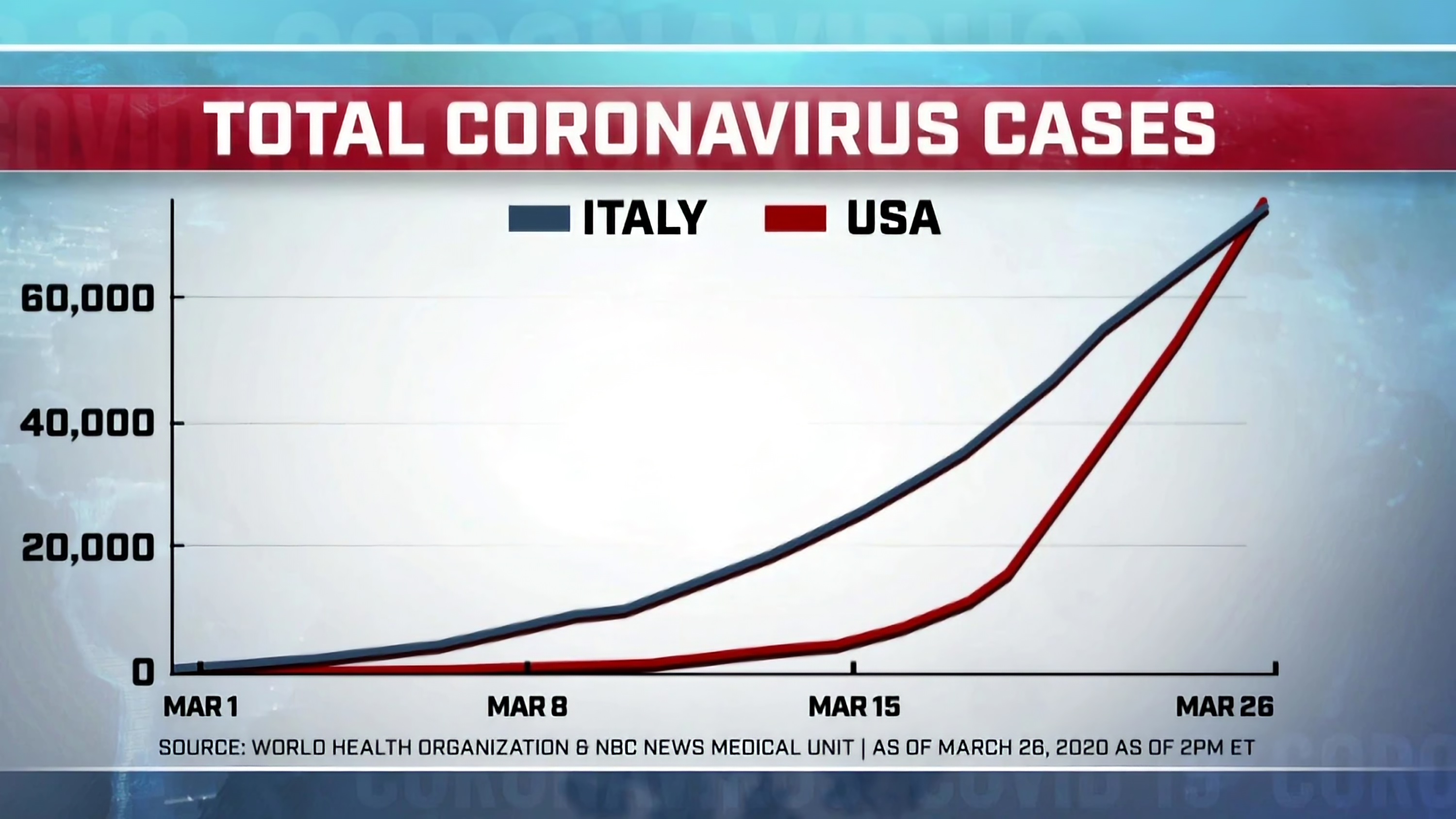
Highlights
◉ Italy overtook China as the country with the most deaths on 19 March 2020.
◉ By 26 March 2020, the United States had overtaken China and Italy with the highest number of confirmed cases in the world.
◉ As of 1 October 2021, Reuters reported that it had estimated the worldwide total number of deaths due to COVID‑19 to have exceeded five million.

INFLUENZA (FLU)
A contagious respiratory illness caused by influenza viruses that infect the nose, throat, and lungs. Since recorded, influenza has caused major global outbreaks at unpredictable intervals. Of these pandemics, the "Spanish flu" in 1918 was the most severe, causing an estimated 20-40 million or more deaths worldwide; less severe pandemics occurred in 1957 and 1968.
Background
Status: Seasonal Epidemics
First discovered: Unknown
Existence: Unknown
Origin: Shunde, Guangdong, China
Outbreak: 1918 Spanish flu (H1N1), 1957 Asian flu (H2N2), 1968 Hong Kong flu (H3N2), 1977 Russian flu (H1N1), 2009 Swine flu (H1N1)
Frequency: 3–5 million severe cases per year
Deaths: >290,000–650,000 deaths per year
Causes
☣
Pathogen
Virus: Influenza virus
Species: Influenza A, B, C & D
Subtypes: H5N1, H1N1, H2N2, H3N2, …
⚗
Transmission
Type of transmission: Airborne & Through Contact
Transmitted through: Respiratory droplets/ aerosols, breathing, talking, coughing, sneezing, contaminated objects/ surfaces
Signs and Symptoms
Incubation Period: 1 - 4 days
Symptoms:
◉ Fever* or feeling chills
◉ Cough
◉ Sore throat
◉ Runny or stuffy nose
◉ Muscle or body aches
◉ Headaches
◉ Fatigue (tiredness)
◉ Vomiting and diarrhoea, especially in children
*Not everyone with flu will have a fever.
Diagnosis
◉ Any of the symptoms
◉ Tested positive using:
Rapid influenza diagnostic tests (RIDTs)
Nucleic acid-based tests (NATs)
Viral cultures
Prevention and Treatment
Prevention
◉ Yearly vaccination
◉ Avoid close contact with people who are sick
◉ Cover coughs and sneezes
◉ Avoid touching your eyes, nose, and mouth
◉ Clean and disinfect surfaces and objects that may be contaminated with viruses
◉ Wear a mask in public
◉ Hand-washing and hygiene
◉ Self-isolation
Treatment: Antiviral Drugs
◉ Prescription medicines (pills, liquid or an inhaled powder)
◉ Make flu illness milder and shorten the time you are sick
◉ Prevent serious flu complications
◉ Most effective when started in the first 48 hours after symptoms appear
◉ Ex: Oseltamivir, Zanamivir, Peramivir, Laninamivir, Baloxavir marboxil, etc.
Vaccination
Influenza vaccine (2 types):
1. Inactivated vaccines that contain "killed" (i.e. inactivated) viruses
2. Live attenuated influenza vaccines (LAIVs) that contain weakened viruses
Immunity period: Generally only last through one flu season (about six months long)
◉ Development of seasonal flu vaccine begins many months ahead of flu season
Prognosis and Complications
Prognosis
Self-limiting and rarely fatal
Complications
◉ Pneumonia (inflammatory condition of the lung)
◉ Acute respiratory distress syndrome (ARDS)
◉ Sinusitis
◉ Bronchitis
◉ Bronchiolitis
History
Disease Emergence
◉ It is impossible to know when an influenza virus first infected humans or when the first influenza pandemic occurred. The first convincing record of an influenza pandemic was chronicled in 1510 that began in East Asia before spreading to North Africa and then Europe.

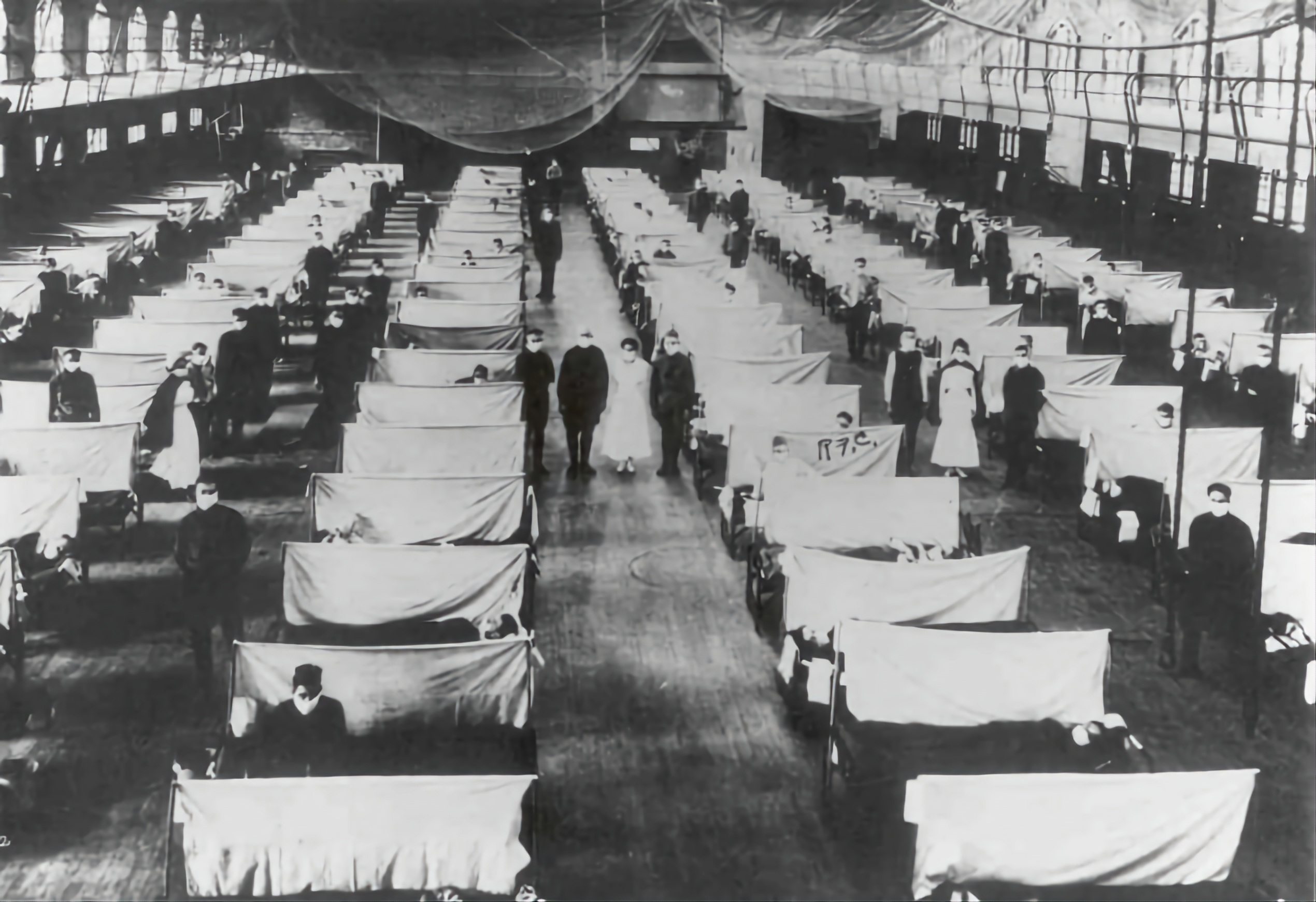
Spanish Flu 1918
◉ The most devastating influenza pandemic and one of the deadliest pandemics in history. The pandemic, probably caused by H1N1, likely began in the USA before spreading worldwide by soldiers during and after the First World War. By the end of 1920, it is estimated that about a third to half of all people in the world had been infected, with tens of millions of deaths.
Discovery of Influenza Virus
◉ In 1931, Richard Shope published three papers identifying a virus as the cause of swine influenza, a newly recognized disease among pigs that was first characterised during the second wave of the 1918 pandemic.
◉ Just two years after influenza viruses were discovered, in 1933, IAV was identified as the agent responsible for human influenza. Subtypes of IAV were discovered throughout the 1930s, and IBV was discovered in 1940.
◉ During the Second World War, the US government worked on developing inactivated vaccines for influenza, resulting in the first influenza vaccine being licensed in 1945 in the United States. ICV was discovered two years later in 1947.
◉ The first antiviral drug against influenza, amantadine, was approved for use in 1966, with additional antiviral drugs being used since the 1990s.
Remarks: IAV-Influenza A Virus, IBV-Influenza B Virus, ICV-Influenza C Virus

Hong Kong Flu 1968
◉ The novel H3N2 strain first emerged in Hong Kong and spread worldwide, causing the Hong Kong flu pandemic, which resulted in 500,000–2,000,000 deaths. This was the first pandemic to spread significantly by air travel.
Swine Flu 2009
◉ Originated in Mexico and resulted in hundreds of thousands of deaths. It was caused by a novel H1N1 strain that was a reassortment of human, swine, and avian influenza viruses.


RABIES
Rabies is present on all continents, except Antarctica, with over 95% of human deaths occurring in the Asia and Africa regions. Dogs are the main source of human rabies deaths, contributing up to 99% of all rabies transmissions to humans. The rabies virus infects the central nervous system of mammals, ultimately causing disease in the brain and death.
Background
Status: -
First discovered: Since around 2000 BC
Existence: At least 5000 years
Origin: Unknown
Outbreak: -
Frequency: -
Deaths: 59,000 per year worldwide
Causes
☣
Pathogen
Virus: Rabies virus
Scientific name: Rabies lyssavirus
⚗
Transmission
Type of transmission: Through Contact
Transmitted through: Bite or scratch from an animal with rabies, saliva of infected animals
Vectors: Dogs, foxes, bats, …
Signs and Symptoms
Incubation Period: 1 - 3 months
Initial Symptoms:
◉ Weakness
◉ Discomfort
◉ Fever
◉ Headache
Progressive Symptoms:
◉ Cerebral dysfunction
◉ Anxiety
◉ Confusion
◉ Agitation
◉ Delirium
◉ Abnormal behaviour
◉ Hallucinations
◉ Hydrophobia (fear of water)
◉ Insomnia
Diagnosis
◉ Fluorescent antibody test (FAT)
◉ Electron microscopy method
◉ Confirmed intra-vitam and post mortem by various diagnostic techniques that detect whole viruses, viral antigens, or nucleic acids in infected tissues (brain, skin or saliva)
Prevention and Treatment
Prevention in pets
◉ Vaccinating dogs, cats, and ferrets against rabies
◉ Keeping pets under supervision
◉ Not handling wild animals or strays
◉ Contacting an animal control officer upon observing a wild animal or a stray, especially if the animal is acting strangely
Treatment: Post-exposure Prophylaxis (PEP)
◉ The immediate treatment of a victim after rabies exposure to prevent virus entry into the central nervous system
◉ Extensive washing and local treatment of the bite wound or scratch ASAP
◉ A dose of human rabies immune globulin (HRIG) and rabies vaccine given on the day of the rabies exposure, and then again on days 3, 7, and 14
Pre-exposure Prophylaxis (PrEP)
Immunity period: Minimum 3 years
Recommended for:
◉ Those who work directly with animals that could have rabies
◉ Those who travel to parts of the world where rabies is common and access to medical care is limited
Way:
◉ A series of rabies vaccine doses are given
Prognosis and Complications
Prognosis
◉ Virtually 100% fatal after onset of symptoms
◉ Vaccination after exposure (PEP) is highly successful in preventing rabies
Complications
◉ Death
History
Disease Emergence
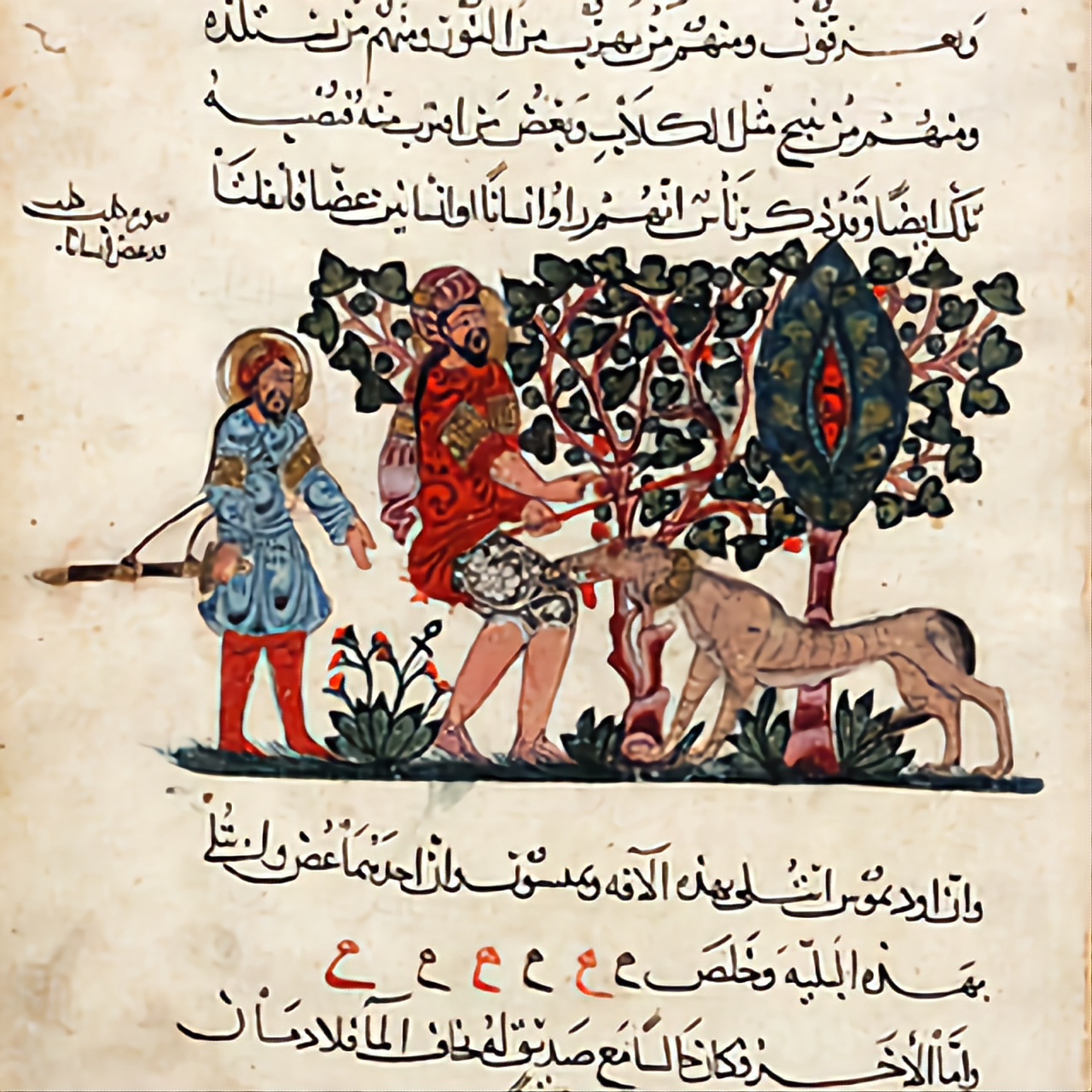
◉ Rabies has been known since around 2000 BC. The first written record of rabies is in the Mesopotamian Codex of Eshnunna (c. 1930 BC), which dictates that the owner of a dog showing symptoms of rabies should take preventive measures against bites. If another person were bitten by a rabid dog and later died, the owner was heavily fined.
Discovery of Rabies Vaccine
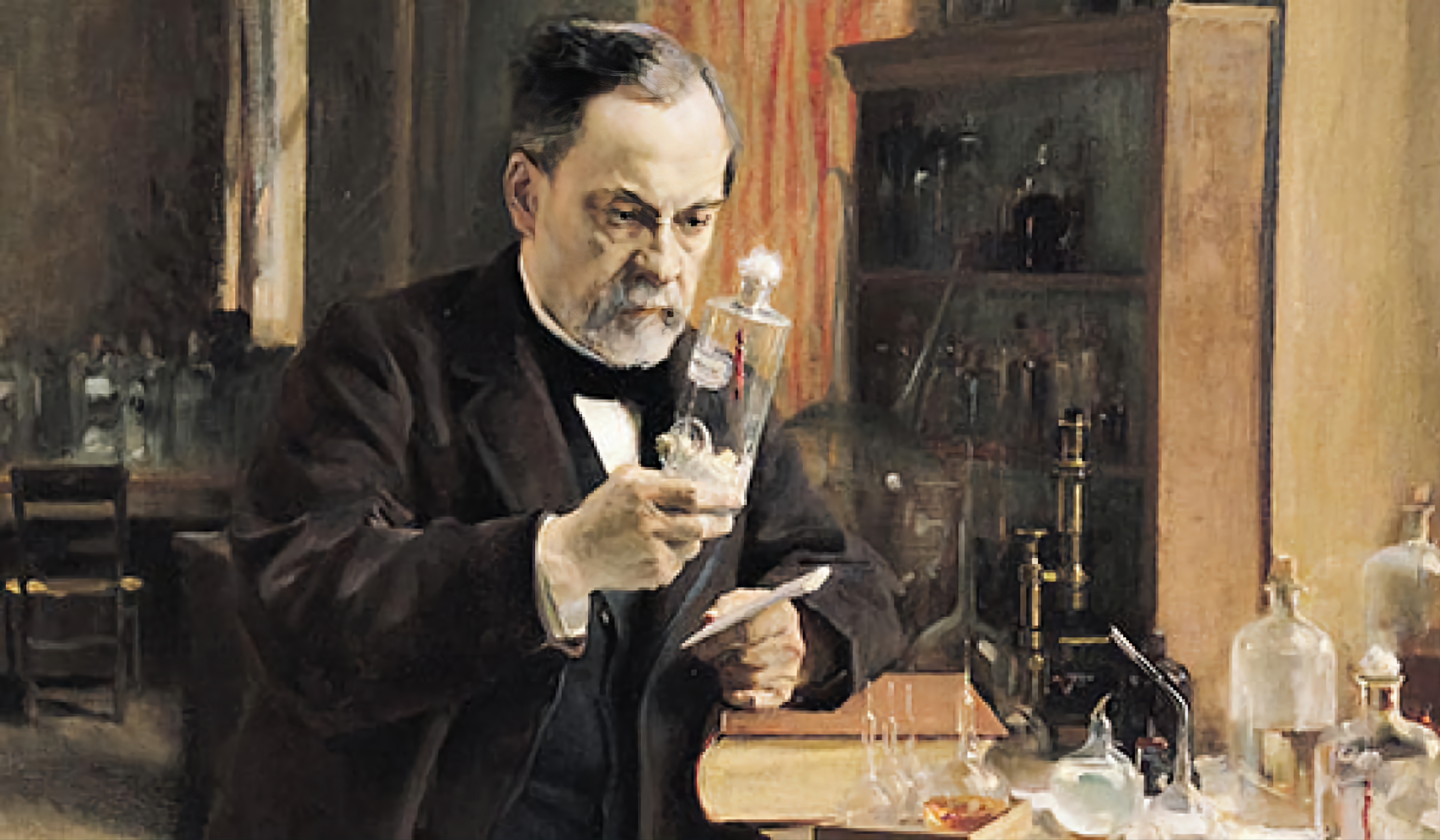
◉ Two French scientists, Louis Pasteur and Émile Roux, developed the first rabies vaccination in 1885. Dr. Louis Pasteur injects a series of a new rabies vaccine into a nine-year-old boy, Joseph Meister who had been bitten by a rabid dog. The boy survives. This is the first vaccine to protect against rabies in people. Before the rabies vaccine, nearly all people infected with rabies died.
A B O U T
Discover
- Smallpox
- SARS
- COVID-19
- Influenza (Flu)
- Rabies
Discover Viruses
A website made to create awareness
Virus Awareness - VA 2022
using
Aligns with the SDG of the UN

 Translate
Translate